This July, Calvary Hospital will begin its new, first-of-its-kind palliative and end-of-life care residency program, in hopes of not only addressing the city’s nursing shortage but also expanding the depths of palliative care.
The residency will invest in an initial cohort of at least eight nurses who will learn at Calvary Hospital and within the organization’s New York metropolitan area home-based hospice program, led by expert Calvary clinician-educators and highly skilled preceptors and mentors.
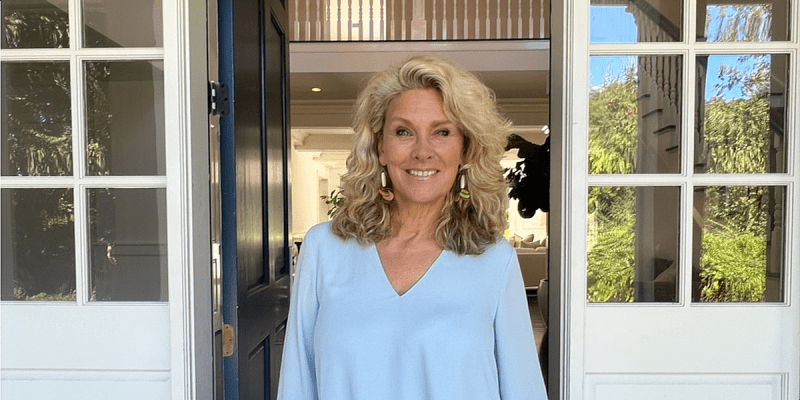
Residency program director Betty Nelson told the Bronx Times that palliative care is one of the quickest growing specialties in nursing, driven by three main factors: the increasing baby boomer demographic, scientific and medical advances that extend our lifespans, and increasing desires among many people to extend life.
By 2050, the number of people living in the U.S. who are aged 65 and older will be 83.7 million, according to the American Academy of Hospice and Palliative Medicine. As the population ages, an increasing amount will be living with serious, complex and chronic illnesses, the U.S. Centers for Disease Control and Prevention states. Medical experts and public health advocates say these demographic changes will require better recruitment and training for the hospice and palliative medicine workforce.

Courses in the program will cover areas such as pathophysiology of diseases, advanced pain management, counseling and communication skills, and advanced care planning. Certification in Palliative Care will be offered through the Hospice and Palliative Nurses Association (HPNA). No other RN residency provides the full spectrum of inpatient and outpatient care that Calvary can provide, Nelson said.
“An important element in recruiting and retaining Registered Nurses, is the level of support they receive when entering a job,” she said. “This is both a recruitment and a retention strategy.”
Meeting that demand is tough. The COVID-19 pandemic’s effect on nurses — which includes burnout, moral distress and unresolved grief from working on the front lines, early retirements among older nurses, and extreme nationwide competition for talent — have led many to leave their jobs, leading to a critical workforce shortage.
“A risk in nursing and any nurse-specialty is excessive and prolonged emotional, physical and mental stress,” Nelson said. “It is associated with our profession. No one is immune from that. Self-care is a critical component of our professional practice and the hospital acknowledges its importance.”
It’s a problem that started long before COVID-19, though.
The New York Times reported on shortages in the 1980s and a state report from 2001 called it an “emerging public protection issue.” A study done by the state Department of Health before COVID found that by 2030 New York state would be facing a shortage of 39,000 nurses.
“It’s a perfect storm forming and leading to a surge in demand for Palliative Care. At the same time, an existing shortage of nurses is projected to continue into the future,” said Nelson. “Just when more registered nurses are and will be needed, there is a very good possibility that there will not be enough. Registered nurses who specialize in Palliative Care will become sought after and will be able to influence and design models of care delivery that are needed to meet an ever-increasing demand.”