The Homecare Savings and Reinvestment Act, sponsored by state Sen. Gustavo Rivera, will eliminate government-funded long-term care (MLTC) plans if it becomes law.
These plans were meant to streamline care and services, such as physical therapy or podiatry, for people with Medicare and Medicaid with long-term medical needs who wish to live at home.
However, while some health advocates have said that eliminating these plans would disrupt care and that MLTCs have a high satisfaction rate among patients, others want to bid good riddance to a system they say needs a major overhaul.
The bill sponsored by Rivera, who chairs the Senate Health Committee and represents the Bronx’s 33rd district, would eliminate MLTCs and transition many patients to a fee-for-service model. Under fee-for-service, Medicaid contracts with home care agencies to pay out separately for each client based on services rendered.
Rivera’s bill can potentially affect a large number of Bronxites, as Bronx County has among the largest and fastest-growing populations of senior adults. Over 300,000 New Yorkers are enrolled in managed long-term care plans, according to 2022 state data.
‘Drive to the bottom’
At issue is the concept of “fully capitated” and “partially capitated” plans as opposed to a fee-for-service Medicaid model.
Under fully and partially capitated plans, a flat fee is paid to the insurance company for each patient covered, regardless of the exact services provided and the cost involved. Rivera’s bill would eliminate all partially capitated plans but preserve fully capitated options.
On the other hand, a fee-for-service Medicaid model would pay out to home care agencies for hours and services provided.
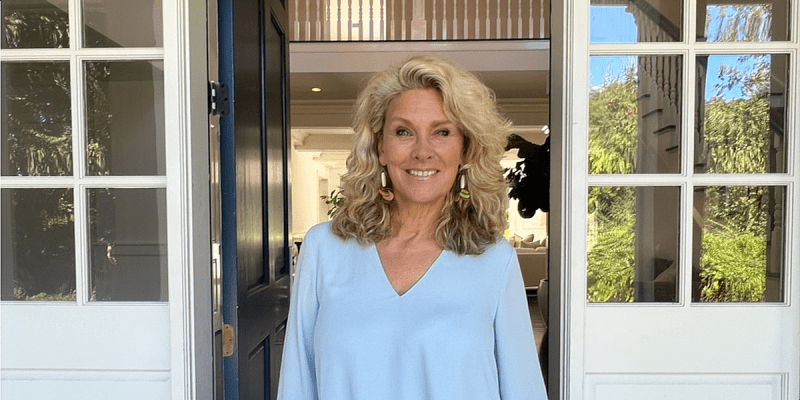
Paula Arboleda, director of health advocacy at Legal Services NYC’s Bronx office, said the capitated model is like a gym membership, with the same amount covering those who use it a little and those who use it a lot.
Under this model, the fee may not cover those who need a lot of care, thus incentivizing insurance companies to approve less — a situation Arboleda constantly sees in her work helping patients appeal those decisions. She called the one-fee system “a drive to the bottom.”
While Arboleda could not comment on Rivera’s specific bill due to Bronx Legal Services’ funding model, she said that the current managed care system is not working.
“We support a model that allows Medicaid recipients to receive medically necessary and lifesaving home care in a timely, accessible way that promotes aging in place. That is not the model we currently have.”
‘High-priced middlemen’
In 2012, it became mandatory for most New Yorkers eligible for Medicare and Medicaid needing over 120 days of long-term home care to enroll in MLTC plans.
Having the state pay for-profit insurance companies to coordinate various Medicaid services was meant to generate savings and create incentives to keep people out of costly nursing homes and hospitals. However, lawmakers in support of the Homecare Savings and Reinvestment Act say the reforms have not worked as intended.
“After ten years of managed care, I’m not convinced that insurance plans are improving care quality or health outcomes,” said Rivera in a statement.
Rivera said that MLTCs run on “high-priced middlemen,” which only make insurance companies richer. According to his bill, the state has paid nearly $6 billion over the past four years in administrative costs and profits to the 24 insurance companies that handle the plans.
If the bill is enacted, Rivera said, “our state will be able to deliver funding directly to the services that New Yorkers rely on and eliminate incentives in the system for corporate profit over improving care.”
He proposes that the savings generated by the bill should be reinvested back into Medicaid and used to alleviate the shortage of healthcare workers. However, some advocates have disputed the amount of savings the bill would generate, saying it is based on flawed data and assumptions.
However, advocates like Arboleda, who has been in the field since before MLTCs became mandatory, say the bottom line is that the current system resulting from the 2012 changes is not working in patients’ best interests.
“The level of care that people are approved for is a lot less than what people were getting before MLTCs became mandatory,” said Arboleda.
She said the vast majority of home care advocacy work at Bronx Legal Services involves helping patients win appeals for more care.
“What we were sold” with MLTCs was care coordination and having a go-to person to assist each client — but “we are not seeing that promise,” said Arboleda.
Instead, she said, “We see really sick people begging” for more care.
‘Managed care never worked’
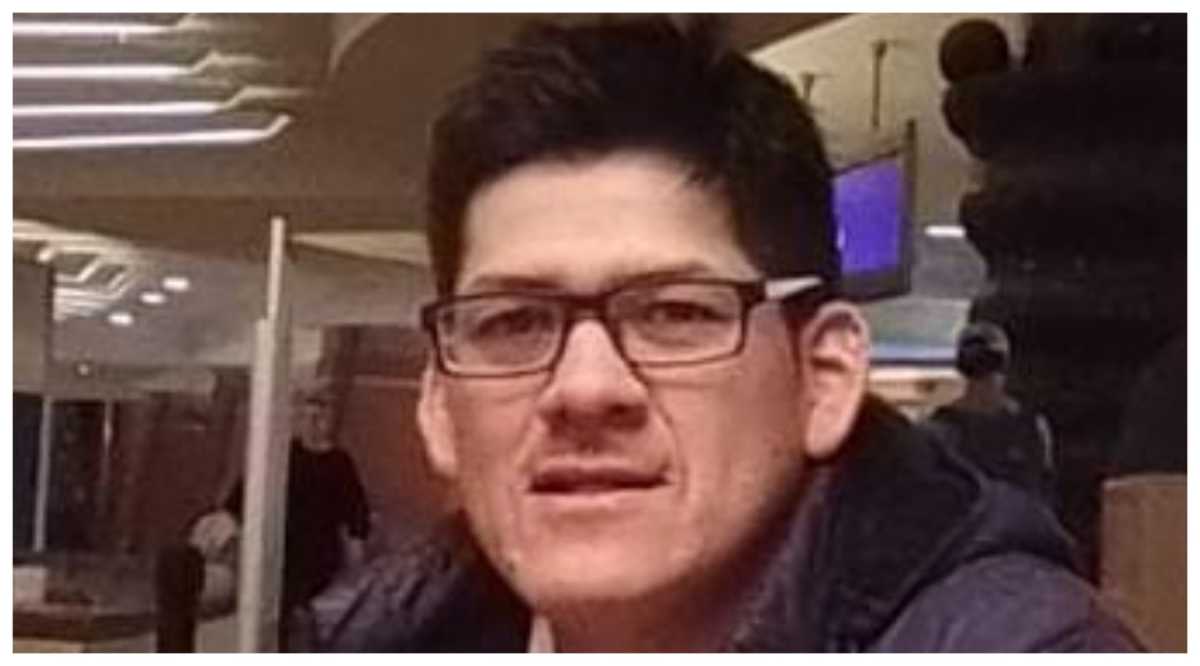
Some advocates who work beyond the Bronx say they have seen the same. With the capitated plan system that includes MLTCs, “There is no incentive to do the right thing,” said Suzanne Paolucci, a social worker specializing in Medicare/Medicaid advocacy and who handles cases throughout New York.
Paolucci said that, in her experience, it is rare for patients to receive the full amount of care they need without going through the external appeal process.
Winning appeals doesn’t come cheap. Paolucci said some clients pay thousands for her help as a private advocate. But she said she virtually always wins her appeals—which she views more as an indication of problems with the system than a testament to her own talents.
If Rivera’s bill passes, Paolucci acknowledged that it would mean fewer clients for her business, but says people would get the care they need.
“Managed care never worked from the get-go,” she said.
Patient advocacy
Just getting the help of an advocate takes a bit of know-how. Many patients don’t know that this type of legal help exists — and some try multiple times to appeal on their own, sometimes over the course of years, before seeking an advocate’s help, said Mul Kim, a staff attorney with Legal Services NYC’s Bronx office.
By the time patients reach her, they are often desperate, she said — and some have already suffered a fall, stroke or some other acute condition that could have been prevented or addressed more quickly if they had help at home.
“They’re not asking [for more care] for the fun of it,” said Kim.
Like Paolucci, Kim and Arboleda say they win all their appeals. “That can’t be a coincidence,” Arboleda said.
While there are some cases of genuine dispute over how much care a client needs, those are rare, according to Kim. Most of the time, Kim said, the client clearly needs more care than their insurance company initially approved — but the set-fee model gives companies no incentive to approve a lot of care.
One of the fortunate ones who found Kim’s help was 77-year-old Lily Jeffers, who lives in the Morris Heights neighborhood of the Bronx.
Jeffers told the Bronx Times she suffers from epilepsy, vertigo, sciatica pain and other conditions, and doctors said her health was worsening, not improving. She had received in-home care from a granddaughter who lived with her, but when the granddaughter moved out in January 2023, Jeffers applied for more care hours and was denied. She then filed an internal appeal — asking the company to reconsider their decision — but was denied again.
Jeffers said she became depressed and anxious to the point where she was prescribed medication. She knew she needed care during basically all waking hours in order to remain in her home.
After her unsuccessful appeal, Jeffers enlisted Kim’s help in filing an external appeal to an independent reviewer. After filing the appropriate documents to support Jeffers’ need for more care, the external appeal was granted. According to Kim, Jeffers was approved for 60 hours of in-home care per week, but the situation took about three months to resolve.
Then, during a Medicare open enrollment period in late 2023, Jeffers switched from a partially capitated plan to a fully capitated plan owned by the same company. Following the change, there was confusion over how many hours she was approved for.
With different staffers saying different things, Jeffers appeared to be at risk of losing 20 care hours per week. Because she switched plans, it looked like her care would be significantly reduced without reason.
“I knew that was incorrect,” she said.
Eventually, Kim proved to everyone involved that Jeffers had been previously approved for 60 hours per week. Although the situation was resolved, Kim said it was an example of inefficiency within the managed care system that caused unnecessary stress and hassle for a very ill person — an example of “the right hand not knowing what the left hand was doing.”
Jeffers now has aides in her home from 8 a.m. until 10 p.m. and said her quality of life is much better.
“I’m not home alone that often,” Jeffers said. “I’m always with somebody now.” She was able to stop taking antidepressants. Her two aides assist with medications, shopping, laundry, showering, doing her hair, cleaning and cooking, she said.
“Everything is getting done as it should’ve been a while ago,” said Jeffers.
But even so, she said she remains on edge, knowing that the relative comfort she now enjoys could be jeopardized due to administrative hassles within the managed care system.
“Even with the advocate, you have to be vigilant,” she said.
Reach Emily Swanson at eswanson@schnepsmedia.com or (646) 717-0015. For more coverage, follow us on Twitter, Facebook and Instagram @bronxtimes