The data is clear. Though we cannot yet predict how any one individual will fare when infected by COVID-19, we do know this: Black, Latinx, and Native American individuals have experienced the highest rates of infection and mortality from the virus to date.
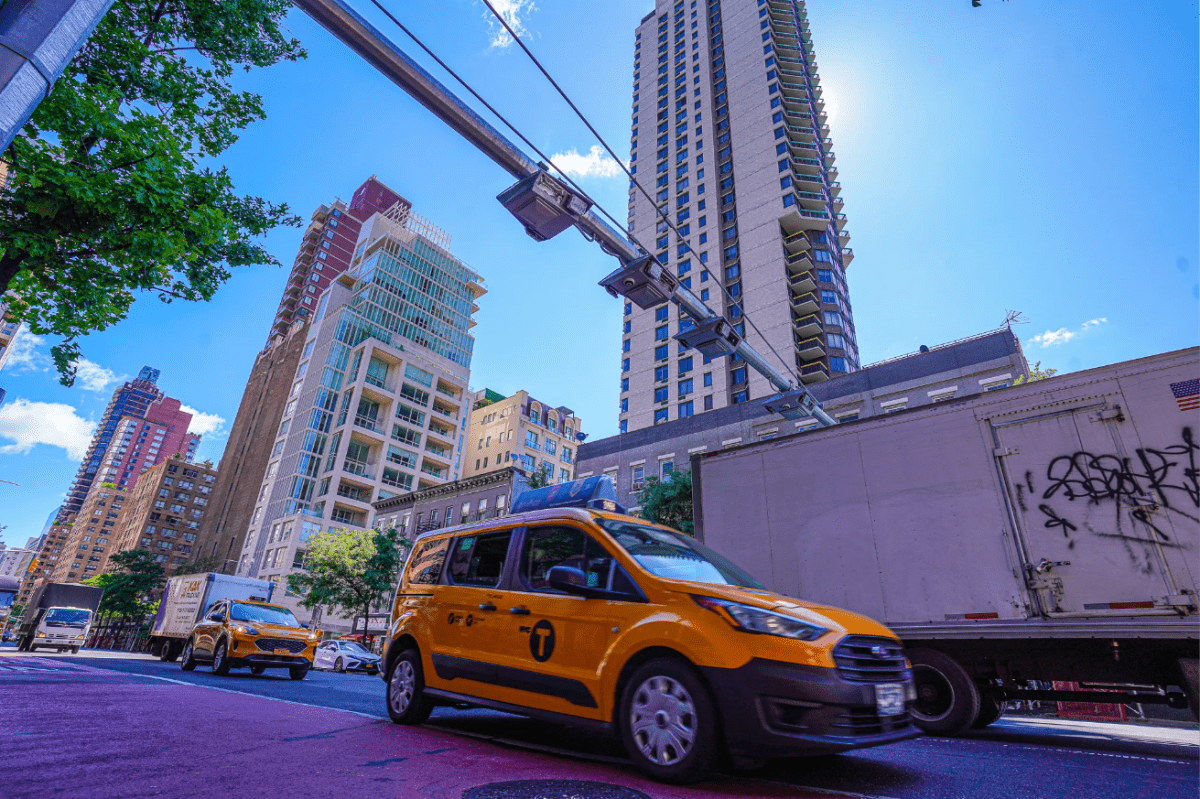
In New York City, where I serve as Chief Operating Officer of Acacia Network, a leading human services provider and the largest Hispanic-led nonprofit in the state, these racial disparities were evident when the pandemic first hit our communities last spring, well before we had any official statistics to back up what we could plainly see here, at the epicenter.
Now, with the COVID-19 vaccination effort underway nationwide, we’ve seen how vaccine access is cutting across lines of race and class, as well. Therefore, it was welcome news when Governor Cuomo and the Biden administration announced this month their new, mass vaccination sites to purposefully target underserved communities.
While these large-scale, pop-up sites are welcome indeed, I encourage New York’s leaders to assist with the swift rollout of the Biden administration’s Community Health Center Vaccination Program and to prioritize the already-existing clinics within these and similar communities.
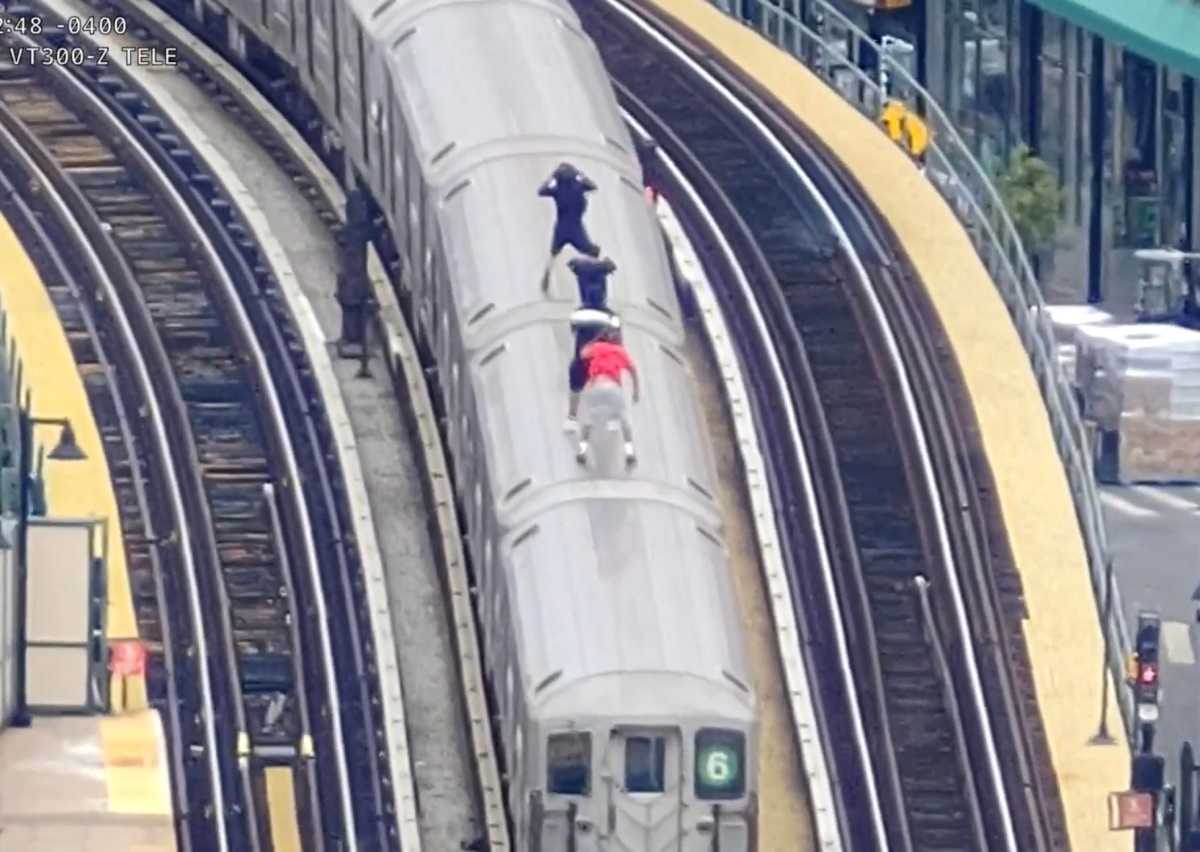
The centers under discussion –Federally Qualified Health Centers (FQHCs)– are uniquely positioned to effectively reach those populations that have struggled to access the vaccine to date: individuals lacking WiFi, a computer, digital skills, English fluency, or ample free time. In many cases, these are the very same groups most vulnerable to COVID-19 and include the elderly, low-income Americans, immigrant communities, and essential workers –often unable to navigate the complexities of securing an appointment online or to travel to a vaccination site outside of their local communities.
Community health centers serve nearly 30 million patients across the country every year, the majority of whom belong to racial and/or ethnic minorities and are living at or below the federal poverty line. They are often at the heart of underserved communities and serve as the go-to source for the health care needs of every member of the family, from newborns to seniors.
FQHCs are able to vaccinate at-risk and underserved communities because we have deep roots in these neighborhoods; residents trust and know us, and we know them. Our leaders and medical providers, from our CEO to the nurses administering shots, live in and reflect the communities we serve, with more than 85% of Acacia Network’s workforce identifying as Black and/or Latinx.
To date, we have inoculated more than 1,300 individuals, over 60% of whom reside in the Bronx.
If New York is to reach those most vulnerable to COVID-19, it must continue to work with the federal government to immediately equip and engage community health centers like ours. It appears now that more supply is soon coming and, with it, a chance to ensure that those who have suffered the worst of this crisis can have equal access to this life-saving measure.